Pre-Analytical Errors and Pneumatic Tubes: What the Evidence Really Says
If you ask ten lab leaders what worries them about pneumatic tube systems, most will give the same answer: "What about pre-analytical errors?"
Concerns about hemolysis, vibration, temperature shifts, and sample integrity have led some hospitals to restrict or even avoid tube transport for key specimens. At the same time, many high-performing labs rely heavily on pneumatic tubes and do not see a spike in errors once systems are designed and validated correctly.
So which is it?
This article looks at pre-analytical errors and pneumatic tubes through a practical lens: what the literature and guidelines say, what risks are real, and how hospitals can validate and manage those risks rather than guessing.
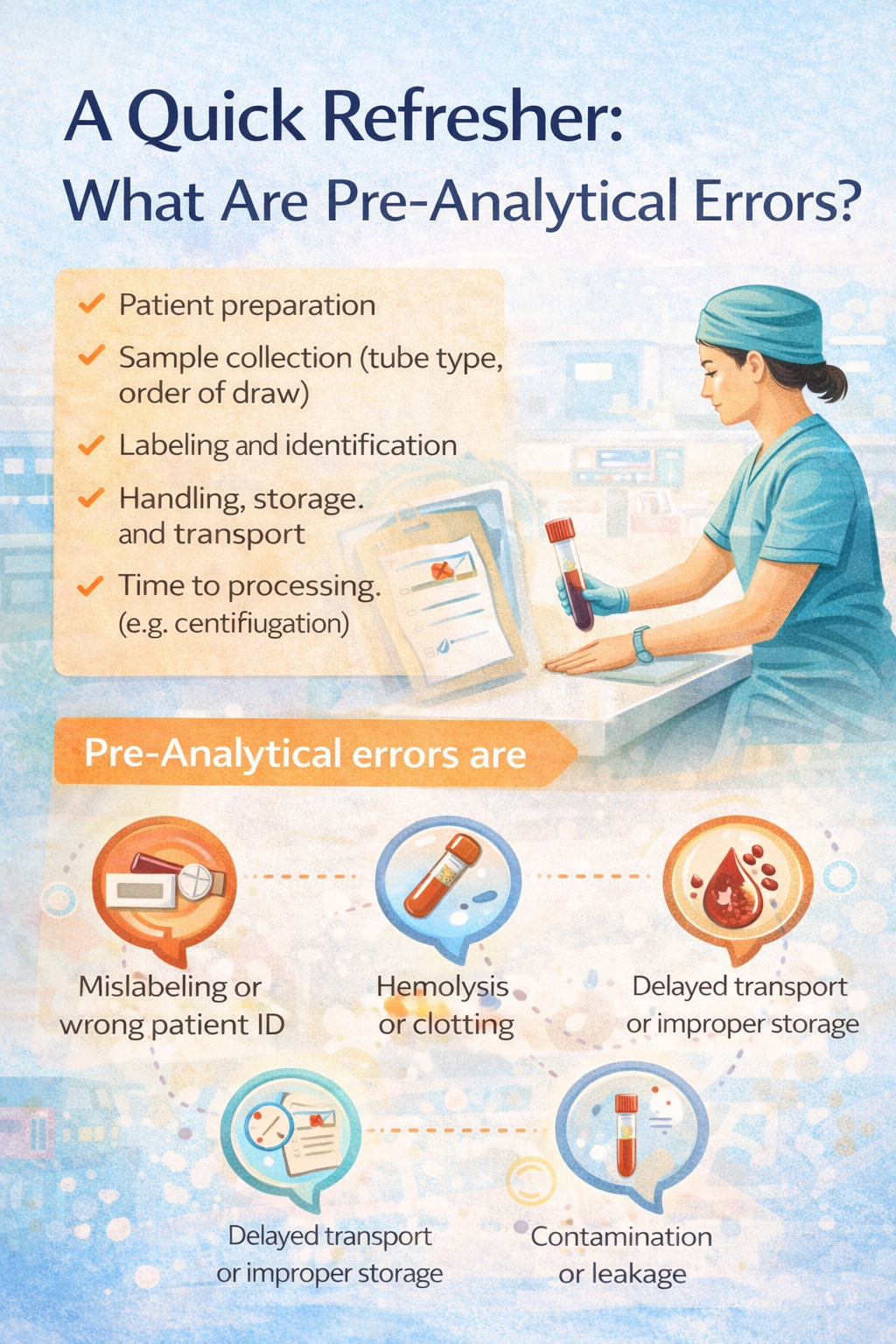
A Quick Refresher: What Are Pre-Analytical Errors?
The preanalytical phase covers everything that happens to a sample before analysis:
Patient preparation
Sample collection (tube type, order of draw)
Labeling and identification
Handling, storage, and transport
Time to processing (centrifugation, for example)
Pre-analytical errors are the most common source of laboratory error. They include:
Mislabeling or wrong patient ID
Wrong tube or incorrect fill volume
Hemolysis or clotting
Delayed transport or improper storage
Contamination or leakage
Pneumatic tube systems intersect this phase specifically at transport and handling, not at collection or analysis.
Why Pneumatic Tubes Raise Pre-Analytical Concerns
Pneumatic tube systems in hospitals move specimens quickly using air pressure. That speed and efficiency also raise specific questions:
Mechanical stress: Do acceleration, deceleration, and vibration cause hemolysis or platelet activation?
Temperature: Does travel through unconditioned spaces materially affect specimen temperature?
Shock events: What happens if a carrier hits a bend, diverter, or station too hard?
Variability: Do different routes, speeds, or system components produce inconsistent forces on specimens?
These concerns are valid, but they're also measurable and manageable.
What the Evidence Says About Pneumatic Tubes and Sample Integrity
Over the last two decades, multiple studies and guidelines have examined the impact of pneumatic tube transport on blood samples and other specimens. While each system and study differs, a few themes emerge.
1. Pneumatic Tubes Are Not Inherently Unsafe
When systems are properly designed for hospital use, operated within recommended speed/pressure parameters, and used with appropriate carriers and inserts, many studies show no clinically significant difference in key analytes between tube-transported and hand-carried specimens for routine chemistry and hematology.
Most issues arise when:
Systems designed for other environments (banks, retail) are repurposed without adjustment
Hospital networks run at high speeds or with harsh routing profiles
Carriers lack adequate cushioning or are overloaded
The configuration and validation matters, not simply the presence of a pneumatic tube system hospital-wide.
2. Hemolysis Is the Main Focus, and It's Controllable
Many studies focus on hemolysis indices and analytes sensitive to red cell destruction (potassium, LDH, AST).
What the literature shows:
On well-designed, validated systems, hemolysis rates for routine samples can be comparable to, or only marginally higher than, manually transported specimens.
Excessive speeds, sharp bends, and poorly cushioned carriers can increase hemolysis risk.
Adjusting route profiles and using appropriate inserts can significantly reduce impact forces.
This is where preanalytical validation is important. Rather than assuming tube transport is unsafe, hospitals can measure hemolysis indices pre- and post-implementation and tune the system accordingly. Without this, hospitals either over-restrict tube use or take risks they can't see.
3. Not All Specimens Are Equal
Most guidance distinguishes between:
Routine chemistry/hematology specimens → often safe for validated tube transport.
Blood products and certain coagulation or specialized tests → may require stricter validation or manual transport policies.
Acceptable specimens to transport via pneumatic tube are usually defined locally, informed by manufacturer recommendations, published literature, and local validation data.
The right answer is rarely "tube everything" or "tube nothing." It's about a clear, validated specimen policy.
How to Validate a Hospital Pneumatic Tube System for Pre-Analytical Safety
The good news: you don't have to guess. You can validate.
Several expert groups and articles (including detailed podcasts and guidelines your team has collected) outline systematic approaches to validation. A robust validation plan includes:
1. Map Routes and Operating Conditions
Identify all relevant routes between collection points and the lab (ED, ICU, wards, OR, clinics).
Document tube diameters, distances, bends, and diverters.
Capture blower settings, speed/pressure profiles, and station impact characteristics.
This helps you choose representative and worst-case routes for testing. Don't test only the shortest, easiest path.
2. Measure Mechanical Stress with the Right Tools
Many experts recommend:
Using a three-axis accelerometer inside a carrier to measure acceleration, deceleration, and shock events along the route.
Recording multiple runs for each route and load condition to understand variability.
What you're looking for:
Peak g-forces at bends, diverters, and arrivals
Differences between "normal" and "worst-case" routes
Whether adjustments to speed, routing, or cushioning reduce peak shocks
This data helps correlate mechanical stress with potential pre-analytical impact.
3. Correlate Stress with Clinically Relevant Changes
Next, you test actual specimens:
Collect paired samples from volunteers or routine clinical draws.
Send one set via the tube system (on representative routes) and another via hand-carry (control).
Analyze both sets for selected analytes and hemolysis indices.
Questions to answer:
Are there statistically significant differences?
More importantly, are differences clinically significant?
Do certain routes or configurations show more risk than others?
If changes are observed, adjust route selection, speed/pressure profiles, or carrier and insert design, then repeat testing as needed.
4. Define and Document Acceptable Specimens
Based on validation:
Create an acceptable specimens list for tube transport (routine chem/hematology, certain coag tests, microbiology specimens).
List specimens/tests that must not be transported via tube (or require special handling).
Build these rules into:
SOPs for nursing, phlebotomy, and lab
Tube station signage and quick-reference guides
Staff training and competency assessments
This turns "we're not sure" into a clear, evidence-based policy.
Pre-Analytical Quality in Day-to-Day Use
Validation is the starting line, not the finish line. Maintaining pre-analytical quality with pneumatic tubes requires ongoing attention.
Monitoring and Quality Indicators
What works:
Track hemolysis rates by source location and transport method.
Monitor rejected specimens and recollection rates over time.
Use LIS data to identify units or routes with higher pre-analytical error rates.
If a particular unit or route shows increased hemolysis or errors after tube implementation, investigate packaging and carrier loading practices, station usage (are staff slamming carriers into stations or overfilling them?), and route assignments and controller logic.
Training and SOP Compliance
Even the best-validated system can fail if carriers are overloaded or improperly cushioned, wrong specimens are sent via tube despite policies, or stations are not emptied promptly, delaying delivery.
Cover in training:
Which specimens can be tubed (and which cannot)
How to package specimens in carriers
What to do when alarms or errors occur
Make sure lab, nursing, and porters all see themselves as part of the preanalytical quality chain.
Atreo's Approach to Pre-Analytical Safety and Pneumatic Tubes
Atreo treats pre-analytical integrity as a core design requirement, not an afterthought.
What that means:
Designing hospital tube systems with routes and profiles that minimize unnecessary shocks and vibration.
Partnering with lab and blood bank teams on validation protocols, including accelerometer testing and paired specimen studies.
Supporting acceptable specimen policies by translating validation results into clear, usable rules for frontline staff.
The result is a system where routine specimens move quickly via tube without compromising quality, high-risk items are managed under clear, validated rules, and pre-analytical questions are answered with data instead of guesswork or fear.
Key Takeaways: What the Evidence Really Says
Pneumatic tube systems are not inherently unsafe for lab specimens. Problems arise from poor design, configuration, and lack of validation.
Hemolysis is the main pre-analytical concern for tube-transported blood samples, but it can be controlled by tuning routes, speeds, and carrier design.
Not all specimens are equal. Hospitals should maintain a validated list of acceptable specimens to transport via pneumatic tube and exceptions that require manual handling.
A robust validation process (combining accelerometer data and paired specimen testing) provides the evidence needed to set safe policies.
Ongoing monitoring of hemolysis indices, rejection rates, and unit-level patterns keeps preanalytical quality on track long after go-live.
Next Step: Schedule a Support Consultation on Pre-Analytical Validation
If your hospital avoids using the tube system for many specimens "just in case," or uses it widely but has never formally validated its impact on pre-analytical quality, you have an opportunity to replace uncertainty with evidence.
Schedule a Support Consultation
We'll:
Review your current tube routes and operating parameters from a pre-analytical perspective
Discuss how to design or refine a validation plan (routes to test, analytes to monitor, tools like accelerometers)
Help you translate results into clear specimen policies that protect patient safety while unlocking tube system efficiency
Frequently Asked Questions About Pre-Analytical Errors and Pneumatic Tubes
Are pneumatic tube systems safe for blood samples?
They can be, when properly designed and validated. Many hospitals safely transport routine blood samples via pneumatic tube systems after verifying that hemolysis and key analytes are not adversely affected under real operating conditions.
Which specimens should not go through a pneumatic tube system?
Policies vary, but common exclusions include some blood products, certain coagulation tests, and very fragile or specialized specimens. Each hospital should define its own list based on literature, manufacturer guidance, and local validation results.
How often should we re-evaluate pre-analytical performance after tube implementation?
At minimum, closely monitor hemolysis and rejection rates in the first few months post-implementation or major changes. Review key indicators periodically (quarterly, for example) or any time you modify routes, speeds, or carrier types. If you see significant changes in pre-analytical error patterns, it's time to re-investigate routes, packaging, and policies.