What Does 'Laboratory Connection' Mean in a Modern Hospital?
Ask ten people in your hospital what "laboratory connection" means and you'll get ten different answers:
"It's how we send samples to the lab." "It's our LIS interface." "It's the hallway between ED and the blood draw station."
They're all partly right.
In a modern hospital, laboratory connection isn't one hallway, cable, or system. It's the way your entire organization connects clinical questions ("What's wrong with this patient?") to the lab answers that guide diagnosis and treatment.
That connection includes:
How orders are placed and labeled
How specimens move physically to the lab
How automation and analyzers receive and process them
How results flow back into clinician workflows
This article unpacks what "laboratory connection" really means today and why it's becoming a strategic concern for operations leaders, not only IT and lab teams.
Beyond the Door: The Lab as a Connected Hub
For years, the lab has been seen as a destination: "We send things there, they test them, and send results back."
The lab is actually a hub in a connected network. Orders flow in from ED, wards, OR, clinics, and virtual visits. Specimens arrive via porters, couriers, or pneumatic tube systems. Results flow back into EHRs, dashboards, alerts, and sometimes external systems.
A strong laboratory connection means:
Fewer handoffs and fewer chances for error
More predictable turnaround times
Better use of automation and staff time
Clear visibility into where delays really occur
A weak connection shows up as:
Lost or delayed specimens
Unpredictable TAT
Duplicate testing and recollections
Frustrated clinicians who feel "the lab is slow," even when analyzers are idle
The Four Pillars of Laboratory Connection
"Laboratory connection" in a modern hospital has four main pillars:
Ordering & Labeling
Physical Transport
Lab Automation & Workflow
Result Delivery & Clinical Use
Each pillar can strengthen or break the connection.
Pillar 1 – Ordering & Labeling: The Digital Front Door
Before anything reaches the lab physically, it's created digitally.
Order Entry and Decision Support
A connected lab starts with:
Clear, standardized order sets that reduce ambiguity.
Embedded decision support to guide appropriate test selection.
Structured priorities (STAT, urgent, routine) that actually drive downstream behavior.
If orders are incomplete, ambiguous, or mis-prioritized:
Specimens may be mislabeled or misrouted.
The lab wastes time clarifying intent.
Clinicians experience avoidable delays.
Bedside Labeling and Identification
At the collection point, orders are pulled directly from the LIS/EHR to label printers. Connections lab to bedside workflows make sure barcodes, patient IDs, and timestamps are consistent. Positive patient identification reduces the risk of mix-ups.
This is the first tangible piece of the laboratory connection: tying the right patient, right order, and right specimen together from the start.
Pillar 2 – Physical Transport: Connecting the Bedside to the Bench
Once collected and labeled, specimens need to move.
This is where many hospitals discover that their "laboratory connection" is really a loose collection of habits. Sometimes nurses walk samples. Sometimes porters pick them up. Sometimes the tube system is used, if someone thinks of it.
A modern laboratory connection treats transport as designed infrastructure, not improvisation.
Laboratory Transport as a System
Transport elements include:
Pneumatic tube systems for fast, consistent movement inside buildings
Porters/transporters with defined, optimized routes
Couriers for inter-building or off-site transport
A connected approach:
Matches item type and urgency to the right transport method.
Uses tube routes for validated specimen types, especially from ED, ICU, and OR.
Keeps nurses and clinicians focused on care, not courier duties.
Read more here: "Laboratory Transport 101”
Eliminating the "Black Hole" Between Collection and Receipt
When lab connection is weak, there's a black hole between "blood drawn" and "blood received in lab."
Strengthening connection means:
Measuring collection-to-receipt times on key routes.
Standardizing when to dispatch (no uncontrolled batching on units).
Making tube use the default for approved specimens where stations exist.
This turns a vague "we sent it" into a traceable, predictable flow.
Pillar 3 – Lab Automation & Workflow: Internal Connectivity
Once specimens reach the lab, the connection continues inside.
Physical and Digital Integration
A modern lab connection links:
Tube stations or receiving points
Pre-analytical stations (sorting, centrifugation, aliquoting)
Automated analyzers and middleware
LIS and quality systems
When everything is connected, specimens are scanned once and tracked across each internal step. Automation can pull work based on real-time demand and priority. The lab can see bottlenecks clearly (pre-analytics vs analyzers).
When it isn't, techs manually move racks without system visibility. STAT labels may not map to STAT behavior inside the lab. Management has limited insight into where time is actually spent.
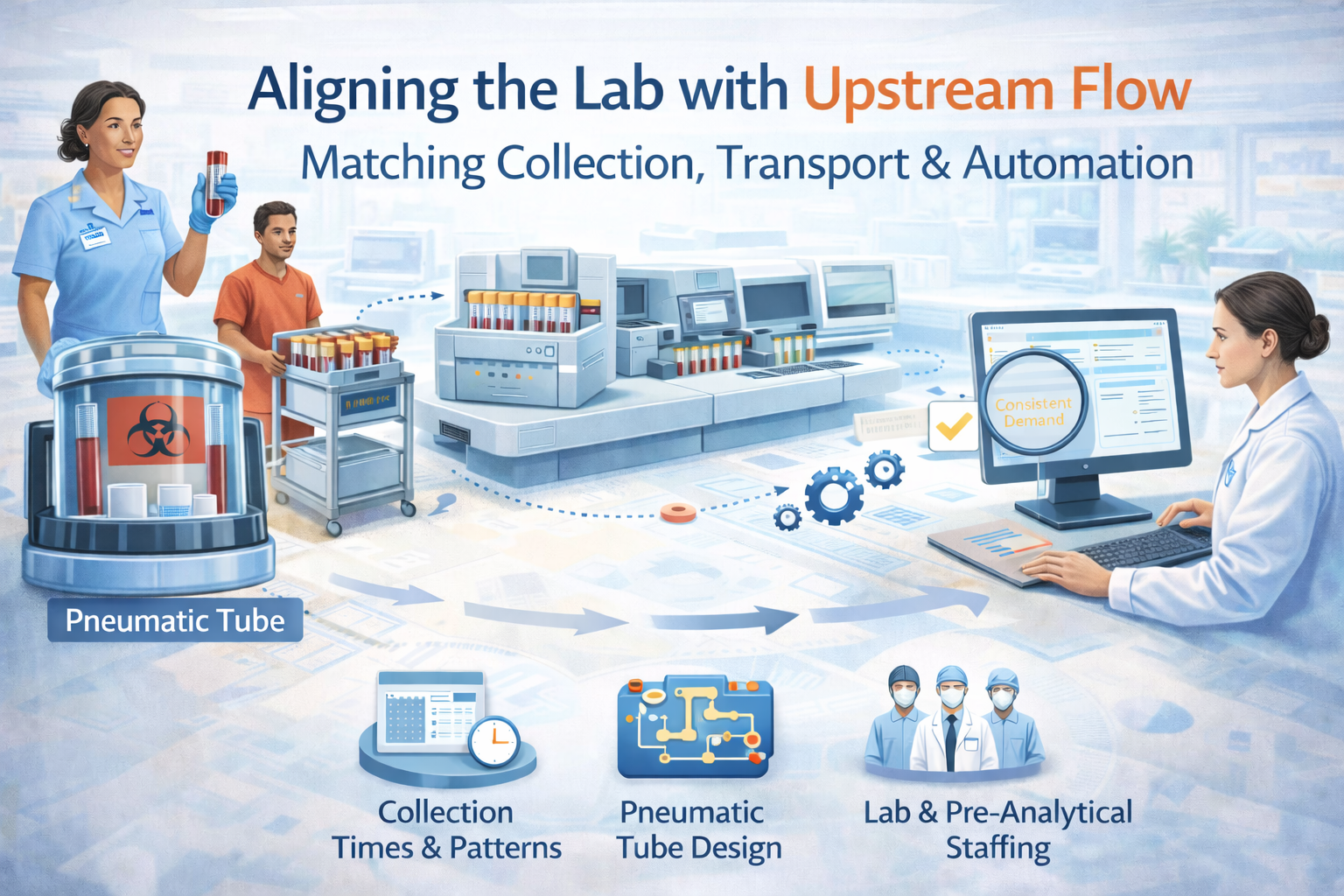
Aligning Automation with Upstream Flow
Even the best automation underperforms if:
Specimens arrive in big, unpredictable batches.
Critical routes to the lab are slow or underused.
Collection and transport practices don't align with automation capacity.
A strong laboratory connection aligns collection times and patterns, transport design (tube, porters), and pre-analytical staffing and analyzer capacity so that work flows smoothly instead of lurching in waves.
Read more here: "How Blood Laboratory Automation Is Transforming Diagnostics."
Pillar 4 – Result Delivery & Clinical Use: Closing the Loop
The last leg of the connection is how results make their way back into clinical workflows.
Seamless Result Delivery
A modern connections lab approach makes sure:
Results flow automatically into the EHR with clear formatting.
Critical values trigger alerts and follow-up workflows.
Clinicians can see final results and status ("received in lab," "in process").
This reduces:
Phone calls to the lab asking "Is that test done yet?"
Duplicate ordering when results are delayed or missed.
Misinterpretation when partial panels are reported.
Making Turnaround Time a Shared Metric
In a connected hospital:
TAT is shared by ED, wards, and operations, not only a lab metric.
Teams look at the entire timeline (from order to result), not analyzer run times alone.
Decisions about staffing, transport, and automation are made with TAT impact visible.
This reinforces that "laboratory connection" is an organizational capability, not a department feature.
Why Laboratory Connection Matters for Operations Leaders
For COOs, CNOs, and other operations leaders, "laboratory connection" is a lever for:
Faster diagnosis and treatment decisions
Shorter ED length of stay and inpatient LOS
Reduced rework and labor waste
Better staff experience (less chasing, fewer "mystery" delays)
Strengthening connection is often more cost-effective than buying another analyzer. You're not asking the lab to work harder. You're removing friction from the whole system.
How to Assess Your Current Laboratory Connection
You don't need a full digital transformation to start. A simple assessment can reveal a lot.
1. Map a Few Key Journeys
Pick 2–3 critical test scenarios:
ED chest pain panel
ICU sepsis labs
Pre-op labs for urgent surgery
For each, map order → collection → dispatch → transport → lab receipt → result. Note who is involved and how long each step takes.
Patterns will emerge:
Units with predictable flows vs units with "black holes" in transport
Places where nurses step in as couriers
Spots where automation waits for work
2. Identify Disconnects Between Pillars
Ask:
Do ordering and labeling align with lab and transport capabilities?
Does physical transport match urgency and volume patterns?
Is lab automation fed consistently, or does it suffer long idle/overload cycles?
Do clinicians receive results in ways that match their workflows?
Disconnects between pillars are where your strongest opportunities lie.
3. Prioritize Practical Improvements
Some examples:
Standardize use of the tube system for certain specimens from ED and ICU.
Implement bedside label printing in units that still rely on manual labels.
Adjust porter routes to align with peak collection times.
Add simple status visibility for high-priority tests in clinical dashboards.
Small changes in connection can deliver outsized TAT and quality gains.
Atreo's View: Laboratory Connection as Infrastructure
Atreo sees laboratory connection as physical + digital infrastructure. Physical: tube systems, station placement, transport routes. Digital: LIS/HIS integration, automation interfaces, tracking data. Operational: policies, roles, and workflows that connect bedside, lab, and back.
Our work with hospitals focuses on:
Mapping real specimen journeys, not only lab processes.
Designing and refining tube networks and transport strategies around clinical pathways.
Helping align lab automation, transport, and ordering practices into a coherent whole.
The goal isn't only a faster lab. It's a more connected hospital where lab insight arrives when and where it's needed.
Key Takeaways: What "Laboratory Connection" Really Means
"Laboratory connection" goes beyond a hallway or LIS interface. It's the full chain from order to result.
Strong connection depends on four pillars: ordering/labeling, physical transport, lab automation workflow, and result delivery.
Weak connection shows up as unpredictable TAT, lost specimens, duplicated tests, and frustrated clinicians, even when analyzers are technically fast.
Operations leaders can improve lab performance significantly by strengthening connection, often without buying new analyzers.
Mapping a few key specimen journeys is the fastest way to see where your lab connection is strong and where it's fraying.
Next Step: Talk with Atreo About Your Laboratory Connection
If your clinicians say “the lab is slow” but your lab team insists analyzers aren’t the bottleneck, you may have a connection problem, not a capacity problem.
Contact Atreo to:
Review how orders, transport, lab workflow, and result delivery work today
Identify where disconnects may be adding delay or risk
Discuss practical options to strengthen your laboratory connection and reduce overall TAT
Frequently Asked Questions About Laboratory Connection
Is "laboratory connection" just an IT issue?
No. IT and interfaces are part of it, but connection spans physical transport, workflows, staffing, and policies. It's an operations challenge that requires clinical, lab, logistics, and IT collaboration.
How is this different from just improving lab automation?
Automation focuses on what happens inside the lab. Laboratory connection looks at the entire journey (from order to result) so you can fix upstream and downstream bottlenecks that automation alone can't solve.
What's the easiest place to start improving our lab connection?
Start where pain is most visible. Map one or two high-stakes test journeys (ED chest pain, ICU sepsis). Measure times and handoffs. Look for quick wins in transport (tube use), labeling (bedside printing), and status visibility. Small, well-chosen changes can dramatically improve the perceived and actual performance of your lab.