How Much Does a Hospital Pneumatic Tube System Really Cost Over Its Lifetime?
When leaders ask, "What's the pneumatic tube system cost?", they're rarely just asking for a number on a quote.
They're really asking:
What will this hospital pneumatic tube system cost to install, run, and maintain over 10–20 years?
How does that compare to doing nothing—or to hiring more people instead?
Will the system still make sense financially as labor markets, inflation, and care models change?
To answer those questions, you need to look beyond a simple "price per foot" and consider total cost of ownership (TCO). This article breaks pneumatic tube system hospital cost into clear layers and shows CFOs, COOs, procurement, and facilities leaders how to think about true TCO and ROI.
Why "Price Per Foot" Isn't Enough
It's tempting to reduce pneumatic tube system cost to a couple of simple metrics:
Cost per foot of tubing
Cost per station
Those are useful for rough comparisons, but they don't tell you:
How well the network will match real specimen and medication flows
How much nurse and porter time it will actually save
How often it will be used—or bypassed
Two systems with similar pneumatic tube system hospital cost on paper can perform very differently over time:
One is designed around clinical pathways, trusted, and used heavily.
The other is designed around construction constraints, mistrusted, and underused.
From a financial and operational perspective, the better question is:
"What is the total cost of ownership for this hospital pneumatic tube system, and what operating costs will it actually avoid or reduce?"
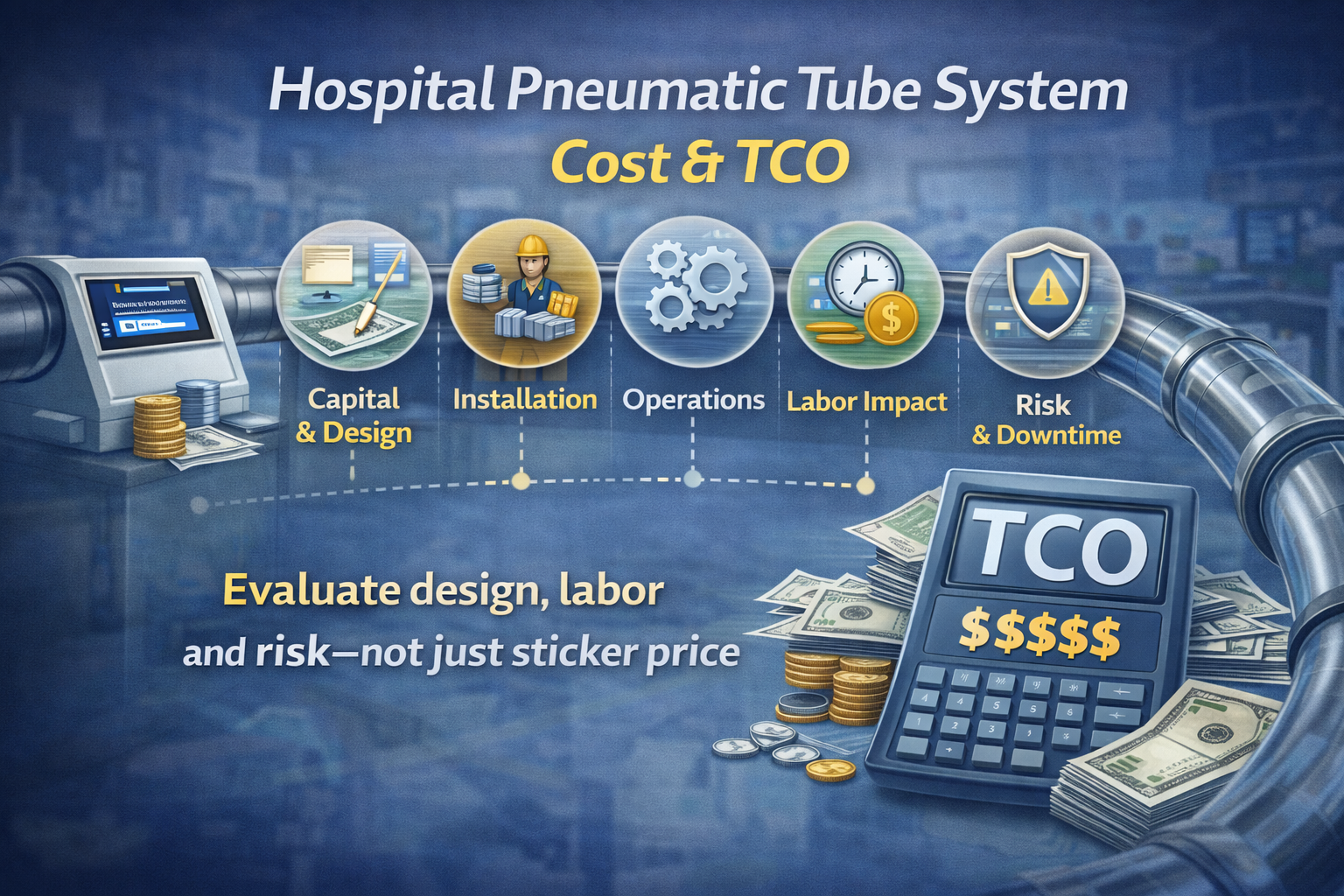
The Five Cost Layers of a Hospital Pneumatic Tube System
Think of pneumatic tube system cost in five main layers:
Capital and design
Installation and integration
Operations and maintenance
Labor impact (staff time and walking)
Risk, downtime, and replacement
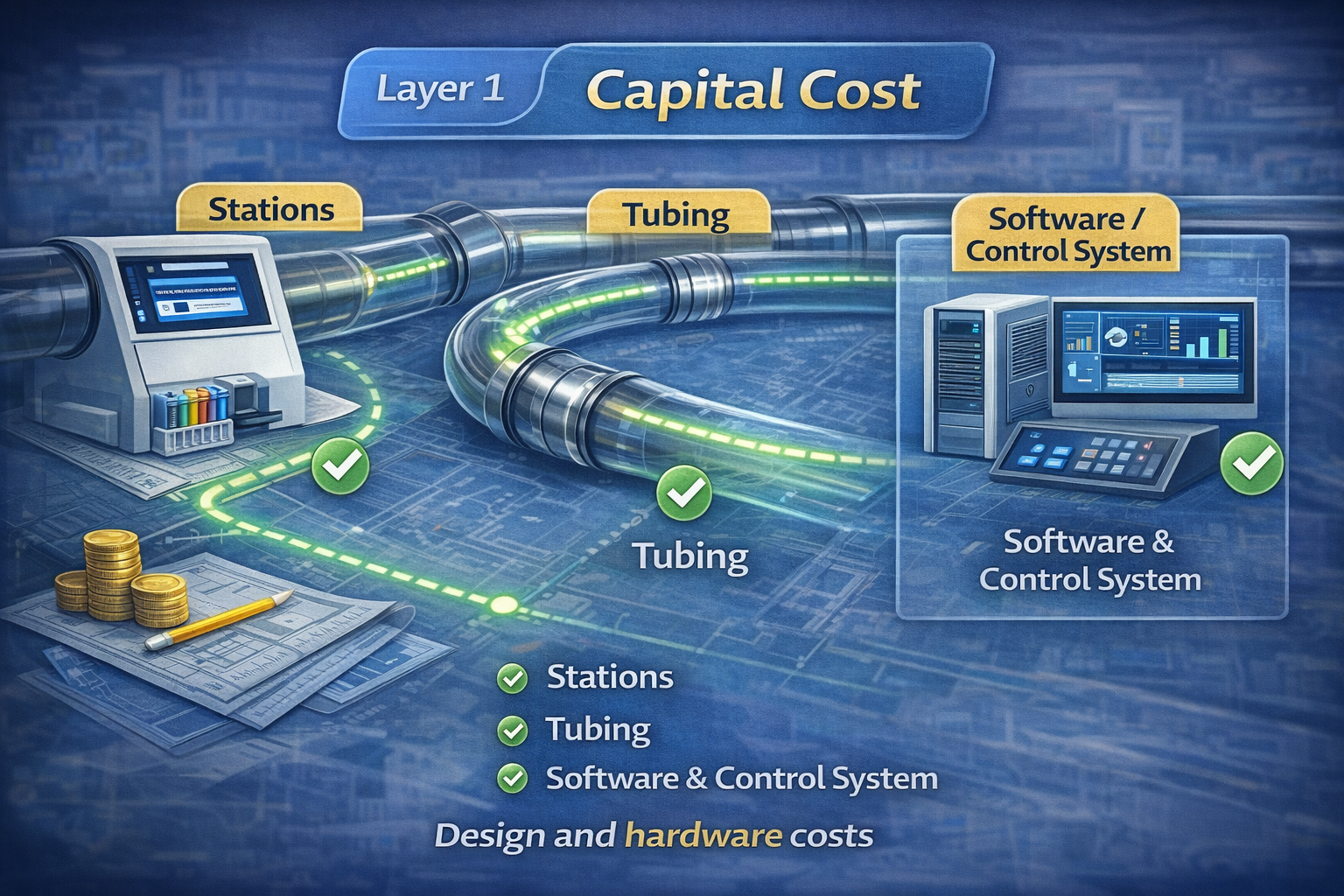
1. Capital and design
This is the visible part of pneumatic tube system hospital cost:
Tubing, stations, blowers, diverters, controllers
Design and engineering fees
Upfront software and interface licenses
Key drivers:
Number and type of stations
Number and length of routes
New build vs renovation vs retrofit
Quality of design (direct routes vs long detours)
Design choices here have long-term financial implications:
Fewer stations can lower upfront cost but increase walking distance and reduce usage.
Thoughtful layouts that align with clinical workflows can increase use and long‑term value.
Read more here "Pneumatic Tube Systems in Hospitals: Design Best Practices for 24/7 Reliability."
2. Installation and integration
Beyond hardware, pneumatic tube system hospital cost includes:
Construction and installation labor
Wall/ceiling penetrations, firestopping, and finishing
Electrical and networking work
Integration with building systems and, when appropriate, with lab or pharmacy systems
This layer is shaped by:
Whether the system is part of new construction or a retrofit
How well facilities, IT, and clinical teams coordinate during the project
Done well, this is a one‑time cost. Done poorly, it leads to rework, delays, and friction that show up later as higher operating costs.
3. Operations and maintenance
Once the hospital pneumatic tube system is live, it becomes part of your 24/7 infrastructure.
Ongoing costs include:
Preventive maintenance and inspections
Repairs to stations, blowers, diverters, and carriers
Replacement parts and consumables
Software/support contracts
Electricity (usually a relatively small share of TCO)
The big drivers here:
System size and complexity
Age and durability of equipment
How proactively the system is monitored and maintained
A system that's used heavily but maintained well can have a lower lifetime pneumatic tube system cost than a cheaper system that fails often and forces workarounds.
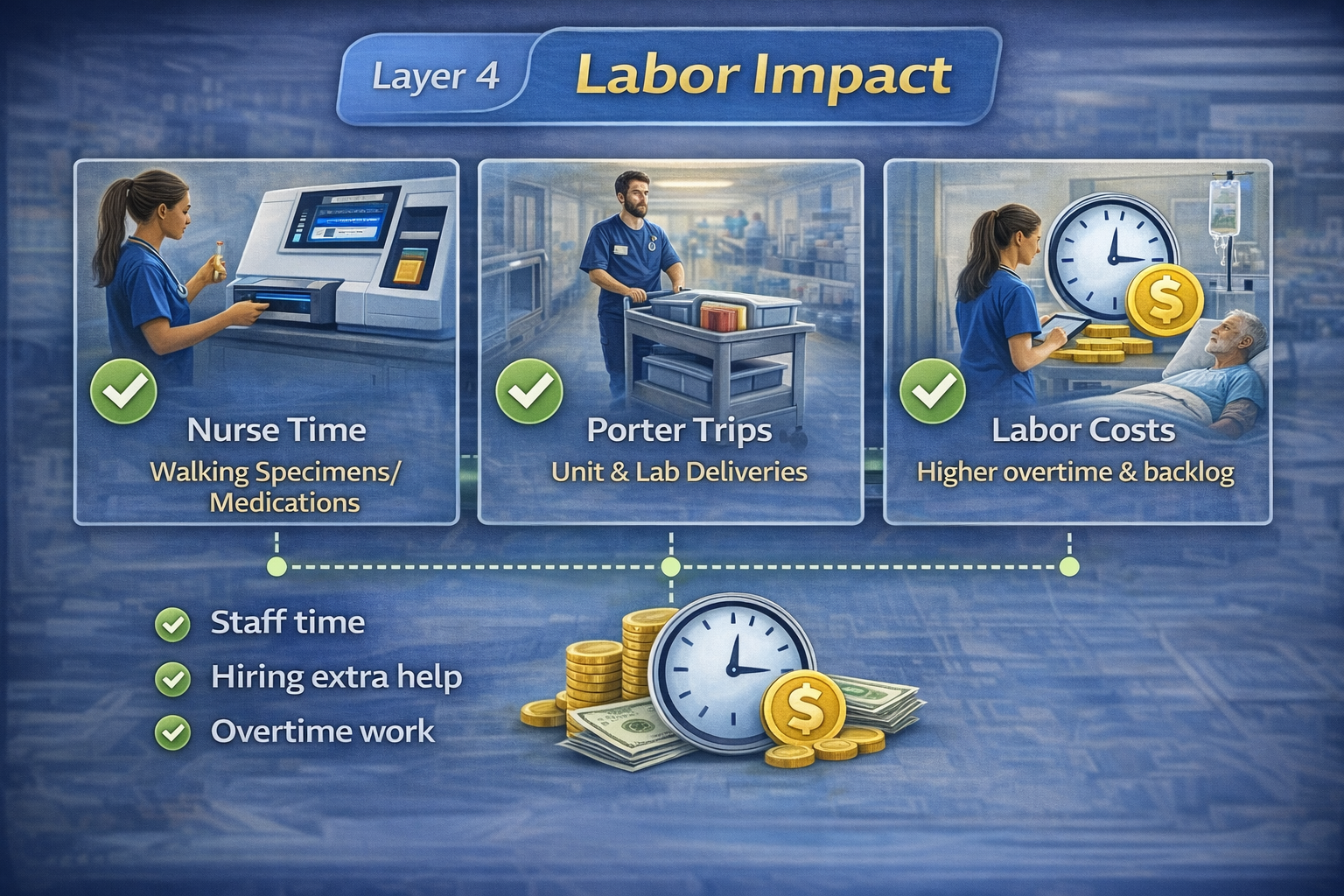
4. Labor impact: the hidden cost line
This is where many TCO conversations shift.
Before a tube system, most hospitals pay for:
Nurses and aides walking specimens and meds to the lab or pharmacy
Porters/transporters shuttling items between units
Extra buffer staffing or overtime when walking and waiting eat into productive time
Those costs show up in:
Nursing and transport salary lines
Overtime and agency spend
Delays that extend length of stay or cause rework
A well‑designed, well‑used hospital pneumatic tube system can:
Replace thousands of walking trips each month
Free nurses to spend more time at the bedside
Let porter roles focus on higher‑value tasks instead of routine shuttling
From a TCO perspective, the question isn't just "What does the system cost?" It's:
"Over 10–20 years, how much staff time and motion will this system realistically replace or prevent?"
5. Risk, downtime, and replacement
Finally, consider:
The cost of downtime (when the system is down and everyone walks again)
The risk of damage, loss, or pre‑analytical errors if the system isn't validated and trusted
The timing and cost of future upgrades or replacements
A low‑bid system that isn't reliable or safe enough to use confidently can:
Increase hemolysis and specimen rejection rates
Delay med or blood product delivery
Erode clinical trust, reducing usage and ROI
In other words, the "cheapest" pneumatic tube system cost up front can become the most expensive option over its lifetime.
Framing tube system cost in CFO/COO terms
To make this actionable for CFOs, COOs, procurement, and facilities leaders, frame decisions around a few core questions:
1. What are we spending now on internal logistics without a tube system (or with a limited one)?
Nurse and aide time spent walking labs and meds
Porter and courier time
Overtime tied to delays and inefficiencies
2. How much of that can a well‑designed hospital pneumatic tube system realistically reduce?
For specimens
For medications
For critical documents or other items
3. Over what time horizon should we evaluate TCO and ROI?
10–20 years is typical for infrastructure.
4. What assumptions are baked into vendor proposals?
Station placement and count
Expected volumes and usage
Service, support, and upgrade commitments
With those answers, you can compare:
The full pneumatic tube system hospital cost vs the cost of "doing nothing"
Different design options vs their projected labor savings and performance impact
Comparing "do nothing" vs a tube system
A simple example to illustrate the thinking (numbers illustrative):
Current state:
Nurses and aides make hundreds of trips per week to deliver specimens and meds.
Porters move items between ED, OR, ICU, wards, and lab.
Average ED→Lab transport time is 10–15 minutes, with wide variation.
With a hospital pneumatic tube system:
60–80% of those trips could shift to tubes.
ED, OR, ICU, and high‑volume wards get direct routes to lab and pharmacy.
Transport times become more predictable and shorter.
On a 10‑year horizon, the key question is:
Does the combined capital + installation + maintenance pneumatic tube system cost fall below the avoided staff time + overtime + delay costs?
For many medium‑to‑large hospitals, the answer is "yes"—if the system is designed around real workflows and actually used.
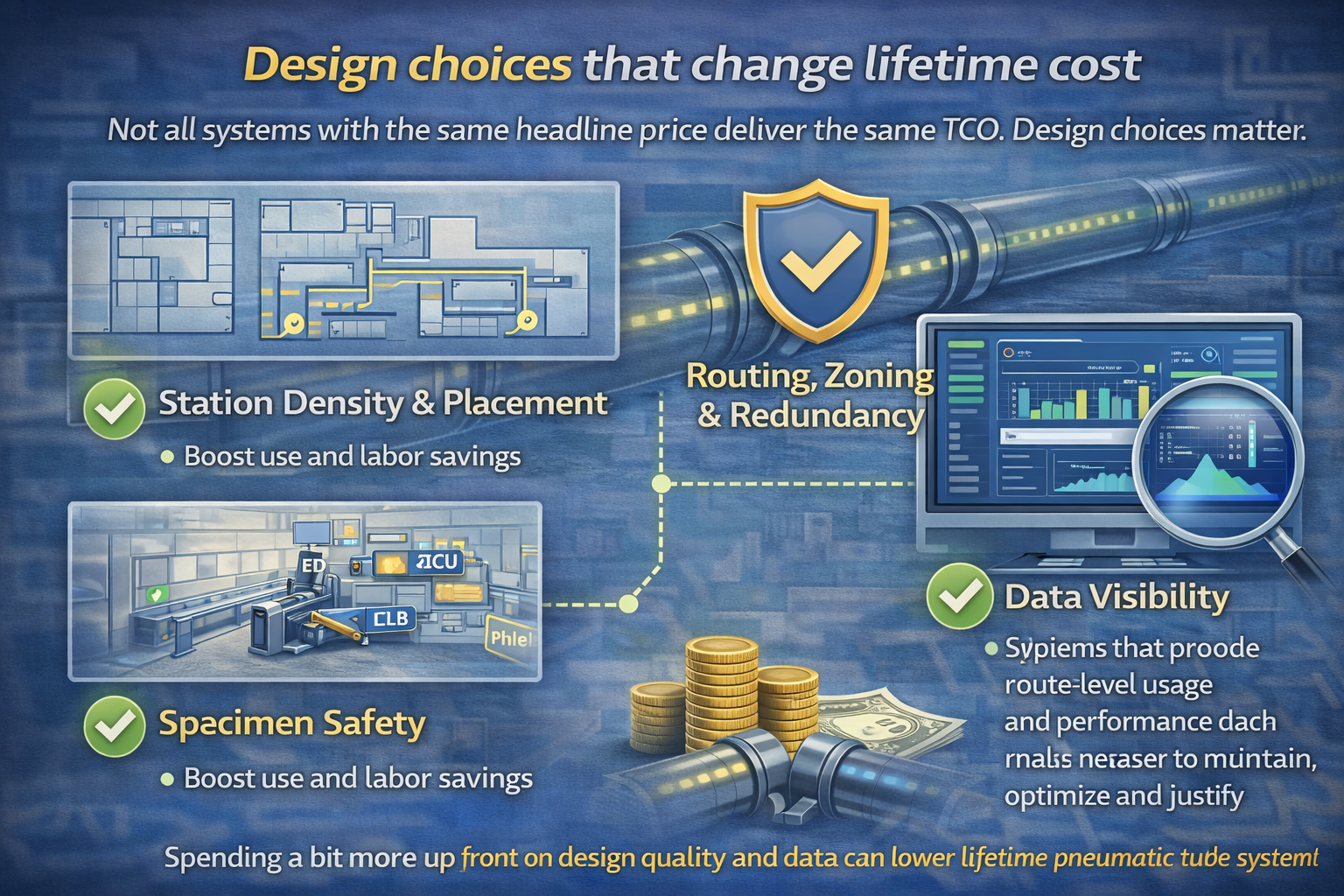
Design choices that change lifetime cost
Not all systems with the same headline price deliver the same TCO. Design choices matter.
Consider:
Station density and placement
Too few stations may lower upfront cost but increase walking and reduce usage.
Stations placed near real work areas (nurse hubs, phlebotomy areas, lab accessioning) boost use and labor savings.
Routing, zoning, and redundancy
Investing in robust routing and zones can reduce downtime and accommodate future growth.
Data visibility
Systems that provide route‑level usage and performance data make it easier to maintain, optimize, and justify the investment.
Spending a bit more up front on design quality and data can lower lifetime pneumatic tube system cost by avoiding rework, underuse, and unexpected downtime.
Atreo's perspective on pneumatic tube system cost and TCO
Atreo treats pneumatic tube system hospital cost as a lifecycle decision, not just an equipment purchase.
In practical terms, that means:
Starting with a clear picture of current internal logistics and labor use
Designing the hospital pneumatic tube system around actual specimen, medication, and document flows
Modeling both capital and operating costs against realistic labor savings and performance gains
Helping hospitals monitor usage and system performance over time so TCO stays aligned with expectations
For finance and operations leaders, that provides a defensible answer to:
Where the money goes
What savings and efficiencies are realistic
How the system fits broader efficiency and inflation strategies
Key takeaways on hospital pneumatic tube system cost
Pneumatic tube system cost includes design, installation, maintenance, labor impact, risk, and future upgrades—not just hardware.
A low upfront pneumatic tube system hospital cost can become expensive over time if the system is underused, unreliable, or poorly matched to workflows.
The biggest long‑term savings often come from reduced nurse walking time, more focused porter work, and fewer delays in care.
Evaluating TCO over 10–20 years—and comparing it to the cost of "do nothing"—gives a more accurate view of value.
Design quality and data visibility are as important to lifetime cost as the initial price per foot.
Next step: talk with Atreo about tube system TCO
If you're weighing proposals for a new hospital pneumatic tube system, or trying to understand whether an upgrade or expansion makes financial sense, we can help you look beyond the sticker price.
Contact us to:
Review the full cost layers of your current or proposed system
Compare "do nothing" vs invest scenarios using your labor and volume assumptions
Discuss design options that balance capital cost with long‑term performance and savings
Frequently Asked Questions
How much does a hospital pneumatic tube system cost?
Headline numbers vary widely by size and scope, but pneumatic tube system cost always includes more than just hardware. You need to account for design and engineering, installation, stations and routes, software, and integration. A small network for a single building may be a mid‑six‑figure project; a large, multi‑building hospital pneumatic tube system can reach into the millions.
What drives hospital pneumatic tube system cost the most?
The biggest drivers of pneumatic tube system hospital cost are the number and placement of stations, the length and complexity of routes, whether it’s new build vs retrofit, and the level of redundancy and zoning you require. Design quality matters: a slightly higher upfront cost for better routes and stations can lower lifetime labor and maintenance costs.
What is total cost of ownership (TCO) for a tube system?
TCO includes five layers: capital and design, installation and integration, ongoing operations and maintenance, labor impact (how much staff walking time it replaces), and risk/downtime costs over 10–20 years. Evaluating pneumatic tube system cost over its lifetime—and comparing it to the cost of “doing nothing”—gives a more realistic view of value.
How do tube systems save money on labor?
A well‑designed, well‑used hospital pneumatic tube system can replace thousands of nurse and porter trips per month. Over years, that can reduce overtime, free nurses for direct care, and let transport staff focus on higher‑value work. The goal isn’t always cutting headcount; it’s avoiding extra positions and overtime as volume grows.